This page is a quick reference for doctors from multiple specialties, who may want to know more about ordering and using genomic tests in Victoria.
Please note: This information is not intended to replace advice from a genetics expert. You can seek advice from clinical genetics services in Victoria and a register of genetic counsellors.
How to order a genomic test | How to use a genomic test

How to order a genomic test
- When should I order a genomic test?
- Which genetic or genomic test should I order?
- Do I need to test the patient’s blood relatives too?
- Is genomic testing covered by Medicare?
- How do I order a genomic test in Victoria?
- Why do patients need to consent to a genomic test?
This page mostly covers testing for inherited (germline) conditions. See our Genomics for oncologists page for genomic testing of cancers.
When should I order a genomic test?
Genetic and genomic tests can be very useful in diagnosing rare and complex conditions, especially when a patient’s symptoms match more than one condition.
Reasons for ordering genomic tests can include:
- a patient with broad and seemingly unrelated health issues
- a patient having a family history of the same health issues
- when there are multiple potential genetic causes for the health issues
- identifying more precise treatment for some cancers
Consulting with geneticists or other medical professionals with genomics expertise can help you decide if genomic testing is right for your patient.
Find out more:
- Support services for paediatricians and nephrologists in Victoria.
- Six real-life case studies show how a genomic diagnosis has informed patient care.
Which genetic or genomic test should I order?
At present, no single genetic or genomic test can reliably detect every type of genetic variant. So the test (or tests) you select for your patient should be guided by what you’re looking for.

A chromosomal microarray looks for changes in whole chromosomes, including duplications and deletions. It’s a useful first-line test for some conditions, including intellectual disabilities.
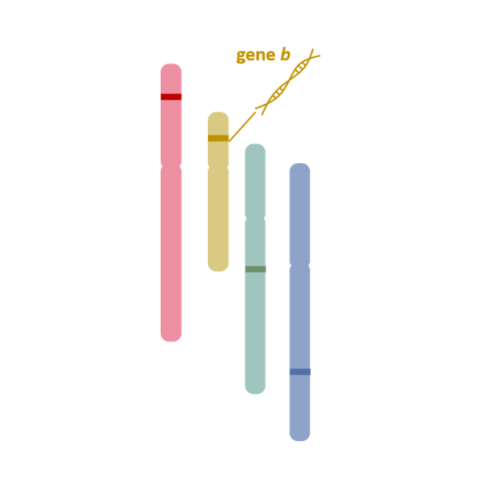
Single gene tests look for small changes or variants in specific genes.
Genomic testing goes a step further, sequencing thousands of genes or a person’s entire genetic code to identify changes that can cause disease. This can enable specific diagnosis of complex conditions, especially when features match more than one condition. Genome sequences can also be stored and reanalysed as more information becomes available over time.
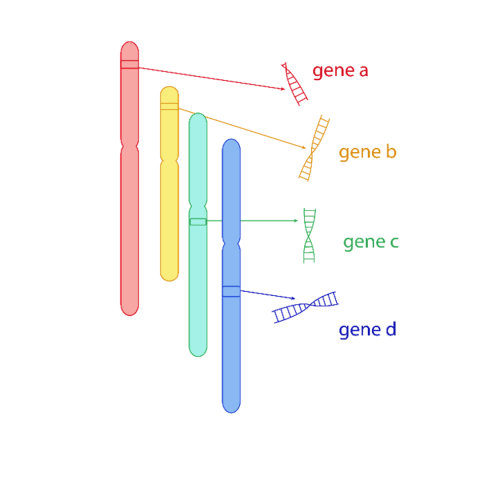
Multigene panels can cover hundreds of genes. This is a relatively fast and cost-effective ways to diagnose conditions when a list of genes linked to the condition is known.

Exome sequencing determines the genetic sequence of all exons, which are the protein-coding regions of the genome. These make up 1-2% of the genome.
Genome sequencing covers both coding and non-coding regions of the genome, including mitochondrial genes.
Do I need to test the patient’s blood relatives too?
Knowledge of a patient’s family medical history can be very important in genomic testing.
A singleton test involves only the patient. A trio test involves the patient and both their biological parents and can provide answers more quickly, as genetic experts are able to determine if genetic variants are new or inherited by comparing results. A duo test includes the patient and one parent.
While it will not always be possible to test a patient’s biological relatives, NHS England’s Genomics Education Programme has a good explainer of the value of trio testing.
Is genomic testing covered by Medicare?
Medicare covers genomic testing for a few specific conditions.
As of February 2024, nine disease areas have Medicare Benefits Schedule (MBS) items:
- Breast cancer (item numbers 73296, 73297)
- Cardiac rhythm disorders (item numbers 73416, 73417, 73418, 73419)
- Cardiomyopathies (item numbers 73392, 73393, 73394, 73395)
- Complex childhood syndromes (item numbers 73358, 73359, 73360, 73362, 73363)
- Deafness (item numbers 73440, 73441, 73442, 73443, 73444)
- Haematological malignancy (item numbers 73445, 73446, 73447, 73448)
- Kidney disease (item numbers 73401, 73402, 73403, 73404, 73405, 73406)
- Mitochondrial disease (item number 73456, 73457, 73461, 73462)
- Neuromuscular disorders (item numbers 73422, 73423, 73424, 73425, 73426, 73427, 73428, 73434)
Please refer to individual item numbers on MBS Online for specific eligibility criteria.
How do I order a genomic test in Victoria?
Genomic testing is available in Victoria through some public and private pathology providers. A pathology laboratory must be accredited by the National Association of Testing Authorities (NATA) to offer exome or genome sequencing.
If you need help deciding which test is appropriate for your patient, the laboratory will often have a geneticist on staff to provide advice. Consultation with a clinical geneticist may also be a requirement for some Medicare-funded tests.
The Human Genetics Society of Australasia has a list of clinical genetics services across the region.
You will also need:
- a blood or saliva sample from your patient
- informed consent from your patient or their guardian (see below)
- a completed order form detailing the test you require. Here is a form used by Victorian Clinical Genetics Services, a major provider of genomic testing in Victoria.
Are you a paediatrician? Here’s a step-by-step guide.
Are you a nephrologist? Here’s a step-by step guide.
Why do patients need to consent to a genomic test?
A genomic test has several features that makes it different to tests that patients may be used to (such as x-rays or standard blood tests). It is important that patients understand these features and their implications.
- A genomic test can have implications for a patient’s blood relatives.
- It can inform future decisions about having children.
- It may show unexpected family relationships if other family members are tested too.
- It can detect genetic changes (variants) which have an uncertain meaning.
- It may even have implications for a person’s life insurance.
In addition, genomic data can be stored, reanalysed in the future, and shared with other laboratories. As research yields regularly new insights about gene variants, reanalysis of genomic data may find answers that were not available before.
For these reasons, it is vital that patients (or their parents or guardians) understand the meaning of having a genomic test and the implications of receiving test results, and provide documented informed consent before the test can be undertaken.
Some useful resources on informed consent for genomic testing:
- A guide on informed consent for health professionals
- Consent forms for adults and parents/guardians of children
- A fact sheet on informed consent for patients
- A fact sheet on insurance and genetic testing
How to use a genomic test
- How is a genomic test conducted?
- What will a genomic test report show?
- What do the terms pathogenic, benign and VUS mean in genomic testing?
- How can I use a genomic test result in patient care?
- How do I explain genomic test results to patients?
How is a genomic test conducted?
A genomic test involves several steps. It begins with a blood, saliva or tissue sample which is sent to a laboratory. The sample is sequenced to obtain the patient’s unique genetic code. The extent of sequencing is determined by the type of test (for example, an exome test will only sequence the exons, or protein-coding parts, of the genome).
The DNA sequence is checked for quality and compared to a reference genome to identify variants. An expert team then reviews the variants and classifies them according to available evidence. The team prepares a report on whether a variant has been found that can explain a patient’s health issues.
Here’s a simple step-by-step explainer of genomic testing.
What will a genomic test report show?
Every lab has its own layout for a genomic test report, but reports include much the same content.
- Whether a variant was found that could explain a patient’s condition. This will be called a pathogenic or likely pathogenic variant. (See below.)
- Whether the patient has one or two copies of that variant in their genetic code.
- Whether the variant identified is new (de novo) or inherited (it’s only possible to know this if the parents were tested too, known as a trio test.)
- What symptoms or presentations in the patient were consistent with the identified variant.
- Where the identified variant was located – which position, on which chromosome.
- Whether any variants of uncertain significance were identified. (See below.)
What do the terms pathogenic, benign and VUS mean in genomic testing?
When a genetic variant is detected in a test, the terms ‘pathogenic’, ‘benign’ and variant of uncertain significance (or ‘VUS’) are used to describe the variant’s impact.
- A pathogenic variant is disease-causing. The presence of this variant in the patient’s genetic code is likely to explain the health conditions the patient is experiencing. A variant is classified as ‘likely pathogenic’ if there is not enough evidence to show that it explains a disease.
- A benign variant does not cause a disease. It may be completely harmless or even beneficial. Similarly, a variant is classified as ‘likely benign’ if there is not enough evidence to conclusively rule is harmless or unrelated to the patient’s presentation.
- A variant of uncertain significance (VUS) may appear related to a disease or the patient’s presentation but there is not enough evidence to support a classification of either pathogenic or benign.
Medline Plus has a useful explainer on variant classifications.
How do I use a genomic test result in patient care?
A genomic test result may inform changes in patient management, depending on the result and current clinical guidelines.
Detecting a pathogenic or likely pathogenic variant can inform the way a patient is managed. This can include decisions on treatment options or palliative care, future family planning or predictive testing among the patient’s blood relatives.
Variants of uncertain significance are generally not used in care, but may be re-examined in the future as new evidence becomes available.
How do I explain genomic test results to patients?
Communicating genomic test results to patients can be difficult, especially if the test result has life-changing implications. It is important to put time and thought into how the results are explained.
Input from a genetic counsellor can be valuable at this step. Genetic counsellors are trained to help people understand and make decisions about their genetic tests, working closely with the patient’s doctors.
Need a genetic counsellor? Search the register on the Human Genetics Society of Australasia.
Watch: Diagnosis Day is a mini-series about families with genetic conditions.
Episode 3 shows the different impacts of diagnoses that are communicated well and poorly.
